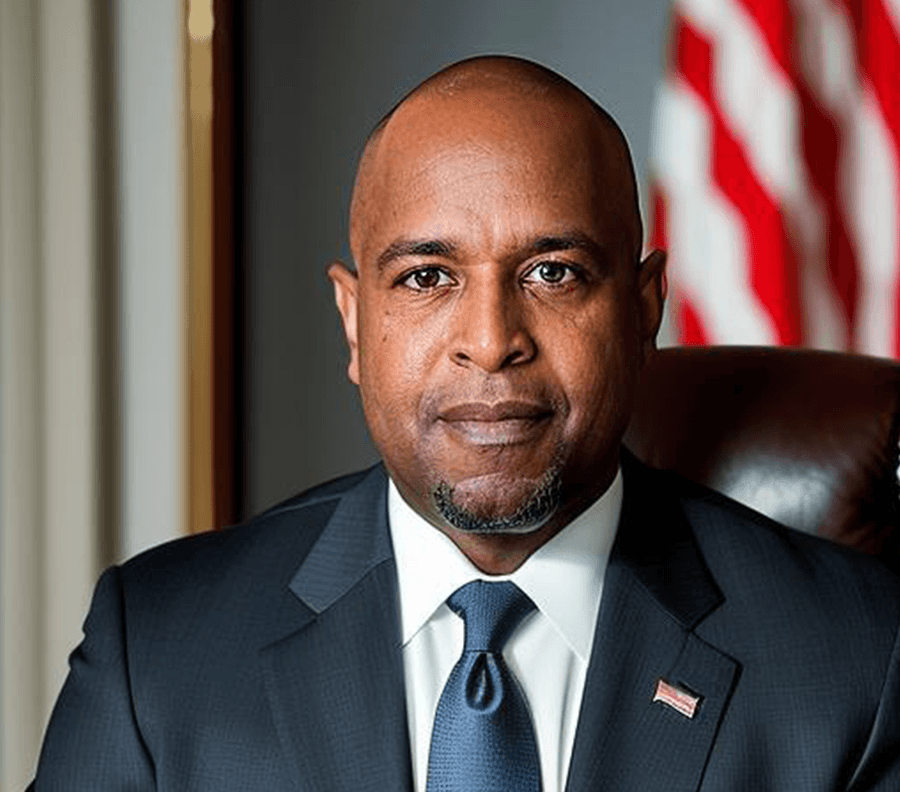
Intro: Are you ready to change your habits, sculpt your destiny, and light up your path to greatness? Welcome to the epicenter of transformation. This is Mick Unplugged. We'll help you identify your because so you can create a routine that's not just productive, but powerful. You'll embrace the art of evolution, adapt strategies to stay ahead of the game, and take a step toward the extraordinary.
So let's unleash your potential. Now, here's Mick.
Mick Hunt: Ladies and gentlemen, welcome heart. Chad and Alicia.
Chad: Thank you. Thank you.
Mick Hunt: You know, on Mick Unplugged, we talk about doing deeper than your why and being fueled by your because. And today, we're gonna talk about a very important cause, fighting a very dynamic and important disease, MPS 1. Chad and Alicia, talk to me about this disease, and then let's talk about how you became a fighter for the awareness of this disease.
Alicia: So MPS one is a genetic disease. It's classified as a lysosomal storage disorder. So in easy to understand terms, our son was born with this. He was born missing an enzyme that breaks down cellular waste, so it affects his entire body. The way that we explained it to our 7 year old daughter at the time was that think of your whole body as a house. Every week, the garbage man comes to pick up the trash. If he didn't, it would just accumulate throughout your house and you would become essentially a hoarder. That's what's happening in his body. His body is not able to break down cellular waste because he is missing an essential enzyme. So instead of being able to recycle it throughout his body and use it, it's accumulating on his bones, his skin, tissues, his organs, and it's affecting everything.
Mick Hunt: So you said something important. It's a genetic disease.
Alicia: Yes.
Mick Hunt: Meaning, both parents are involved, one parent's involved. Talk to us a little bit about the disease and the inheritance of the disease.
Alicia: So in order for this specific type of MPS, there are multiple types. But for MPS one specifically, both parents are carriers. So we both passed on a genetic mutation to him, and we just happened to hit the genetic lottery and find a match that both carried this. Every person carries about 3 to 6 lethal genetic mutations. It's just finding that partner that also carries it and then potentially passes it on. Because we both carry it, there is a 50% chance that we would have a carrier child, which is our daughter, a 25% chance that we would have an affected child, which is our son, and then the 25% chance to have a completely unaffected child and non carrier child.
Mick Hunt: Wow. I'm assuming your son was born and you didn't know he had MPS.
Chad: Right.
Mick Hunt: Walk me through what led you to say, hey. Something's not right. Maybe we need to have testing, and then the moment that you find out what this disease actually is.
Alicia: So we have noticed, you know, some motor skill delays, definitely a speech delay.
Chad: Well, I'm development delay.
Alicia: Just developmentally all around global developmental delay.
Chad: Obviously, we had our daughter first, which was crazy. So we had our daughter first, so there was things that kinda jumped out to us that
Alicia: That she had done earlier that he had not done. He was sick all of the time, like, constant ear infections, sinus infections. We were at the pediatrician's office every week getting antibiotics and they were just like, you know, sometimes kids have weaker immune systems. Like, he had his first surgery when he was 4 weeks old. He had a double hernia repair, inguinal hernia repair. And they said, you know, that's normal specifically in children, sometimes in boys. So everything that we had pointed out to them was explained somehow.
Chad: And then the, like, the development side, they said, oh, he's a boy. He's a boy.
Alicia: He's a second child. You you baby him, like Right. They take longer to develop. All of
Chad: this It's not that they pushed everything off. They just they kinda had an answer for everything, like, hey. He's a boy. He's He's this. This is that.
Alicia: And it wasn't until around the age of 2 that, you know, we went to the pediatrician and they said, okay. He is developmentally delayed. His speech is delayed. The shape and size of his head, like, has anyone ever said anything to you about his head? It's big. So they sent us to Duke to see neurosurgery in July of 2019, and they took an X-ray. They said, nope. He just has a big head. Like, my brother had a big head. So we thought, okay. Well, genetically, like, that runs in our family.
Mick Hunt: Big heads run-in the family.
Alicia: Yeah. It wasn't like he was born with a super small head and it got really big over time. Like, it has always been big. He was £9 8 ounces, which in hindsight is also related. But it wasn't until February of 2020 that we brought him to Wake County Public Schools to be evaluated for special education pre k. And, we had already at that point had a genetics appointment scheduled. We had scheduled that back in November of 2019 after his doctor was like, you know, he's sick all of the time. We have this lingering concern of his head. You know, they said it was fine, but just things are not right. Maybe he has some sort of processing disorder. We think that it would benefit you to find out before he goes into kindergarten if there is something with his learning that would benefit you to know. So we had scheduled an appointment with UNC Genetics back in November of 2019. They could not get us in until May of 2020, but the doctor assured me, we do not think it's anything that needs to be rushed. We don't think it's anything, like, super scary and important. We just think it would benefit each and every before he goes into the school system.
Okay.
Chad: I brought him to the evaluation, and it was pretty hectic.
Alicia: Yeah. So the She couldn't tell me what evaluated with Wake County Public Schools. I almost canceled that appointment because I am very much control free guy who wants to be the one to take him to appointments.
Mick Hunt: Right.
Alicia: He took him. They called me.
Chad: There was 7. Occupational therapy, physical therapy, speech therapy. I mean, you named his therapist. They were in the room just watching what Which is standard
Alicia: for a special education evaluation.
Chad: Okay. But someone first time going into that, it's as a dad, like, she's very well like, she's the type that she looks up, like, everything about it. It.
Mick Hunt: And then
Chad: I'm the type that I just walk in and
Alicia: I'm like, okay. Shows up for evaluation.
Chad: I had 7 people just like, holy cow. Just we're here to watch your kid. Now I was like, okay.
Mick Hunt: A little intimidated. Right?
Chad: It was. It really really was. And then I don't wanna say I don't know how it went and then they called her out.
Alicia: So they so they knew that we had a genetics appointment scheduled. Like, they knew his medical history. They knew all of that.
Chad: 5 months in advance.
Alicia: So he showed up to that evaluation. 1 of the therapists called me a few days later and was like, hey. We know you have genetics scheduled for May of 2020, currently February of 2020. We think you need to move this appointment to as soon as possible. And I'm at work in a position in a full time position that I just started with my job, recently promoted, sitting in my office, about to go meet clients for a walk through of their venue. And I'm like, okay. Like, what did you see in the 2 hours you spent with him that his pediatrician has not seen in the 100 appointments we've been to in the last 2 years? And they didn't really wanna tell me because they're not physicians. I mean, I can respect that. They didn't wanna tell me all this.
Chad: Something that they had to report and then they pushed everything up.
Alicia: So some so some of the things that they had said were, you know, we noticed that his fingers are curled. We noticed that he has an abnormal head size and shape.
Chad: Mobility. Like, and what his arms
Alicia: are like. Range of motion. He has core spatial features. And I'm like, okay. Well, when I get on Google and I Google genetic testing in toddlers, it's giving me a 100 different things. Like, I don't have time to sit and Google all these things. If you're telling me that it's, like, urgent, I need to know what you think you saw. And they thought that they saw Hunter Syndrome, which is MPS 2, and that only affects boys. They said something in the Hunter Syndrome or the Hurler Syndrome family. And I'm like, okay. I've literally never heard of any of those things. So I got on WebMD, I got on Google and did exactly what they told me I shouldn't and I'm like checking off every single one of these characteristics, every single one of these symptoms he has.
Mick Hunt: It was like spot. It was starting to make sense.
Chad: Yeah. Oh, man. It was like Noisy
Alicia: breathing, abnormal head shave, constant sickness, umbilical hernia, inguinal hernia, large
Chad: burp Everything was the boxes were just checking after one another.
Alicia: And I'm like, okay. And then I read life expectancy 10 years old. And I'm like, okay. Well, he's 3. He's gonna be 3 at this point. And I'm like, okay. Well, like, what the heck? Like, what am I supposed to do now? So I called UNC Genetics. I'm like, listen. My appointment's in May. I can't wait till then. I've already been on Google. I've already diagnosed my kid. Like, I went on Google images and typed in Hunter Syndrome, and my kid looks like all of these other kids. Like, clearly, like, I've already diagnosed him in my head.
Chad: Yeah. Like, they all look they almost some of them look like brothers and sisters.
Alicia: Like, he looks like he could be related to all of these children. And, you know, like I said, my brother had a large head, but he never really looked like Chad. He never really looked like me, you know. Now it makes sense. Why? So they were great. UNC Genetics was great. They asked me some follow-up questions like, well, you know, tell me his symptoms. Tell me what stood out to you on WebMD. Like, what characteristics does he have? Mhmm. And they got us in as soon as possible to at least do the diagnostic testing for it. The the doctor was out of the country, but they said if you can come, we can do the the blood sample and the urine sample, which is what they need in order to diagnose. And as soon as we arrived, the genetic counselor was like, do you mind if I take a picture and then send it to the doctor? And as soon as she said that, I knew that she knew that he had it. So we had followed through with the testing. We had an appointment on February 25th. I'll never forget that date because that's the date that he met with the doctor, and they had confirmation at least from the urine test that showed that he had elevated gags, which is that waste that he can't break down.
Mick Hunt: Right.
Alicia: So they could tell us right off the bat, he definitely has MPS. We don't know which type.
Chad: Yeah. There's 1 through 7, so they were like, he's in that Yeah.
Alicia: Once we get the blood test back, it'll confirm. But they looked in his eyes. He has corneal clouting, which is a symptom of MPS one specifically. So the doctor was like, I would be willing to bet that it was MPS one. So, of course, I come in with my notebook full of questions like, okay. Like, what is next? Like, what do we do from here? Because typically, children are diagnosed within the 1st 2 years of life. If their state tests for it through newborn screening, they're diagnosed at birth, which North Carolina did not test at the time. They actually did a screening pilot that ended a week and a half before his birthday. So had he been born a week and a half earlier, we would have known at birth. He would have been able to be treated by 3 months old, and newborn screening saves lives. Like, there's no cure for this disease, but earlier detection leads to earlier treatments, which leads to better outcomes because now he has 3 years of irreversible damage that we can't Correct. Undo because it took so long to get a diagnosis.
Mick Hunt: Mhmm.
Alicia: That is why we are such advocates of this. I have
Chad: see that what we've both been through Yeah. For 4 years or a
Intro: while.
Alicia: No parents should get this diagnosis. Mhmm. But no parents should have to wait 3 years to get this diagnosis.
Mick Hunt: Correct. I was just gonna say, Chad, I wanna come to you for a second. Right? Being a father of a son, it hits differently.
Chad: It's funny you say that.
Mick Hunt: Right? It hits differently. So that moment for you and, you know, I'm not I promise I'm not trying to stir emotions, but I'm kind of emotional hearing this, thinking about it from your from both of your perspectives. What was that moment like that the diagnosis is confirmed and then all the millions of information that's out there that you can read. Right? Like, there's a ton of what if scenarios. For the past couple of weeks, you know, I've been familiarizing myself with MPS y just because of our relationship. Right? Like, what was that moment like for you?
Chad: So it's funny you think, like, the dad in it is always, like, the tough one that gotta get it done. We're gonna get through this. Polar opposite, like polar opposite. Like I was the grieving one and maybe I don't wanna say if it was my daughter, it'd be different. Probably still be the same. But it's like what was going through my head was like, that's your son. That's the person that's gonna carry on with your family name. Right. I grieved like hard, like real hard. And she went right to the grindstone. I was like, all right, we're gonna do this. This is what we're gonna do.
Alicia: It's like, I need to learn as much as I can. I need to
Chad: quit myself. Yeah. Yeah. And it it turned hard at that point because I was grieving and she wasn't.
Alicia: I wouldn't say I wasn't. No.
Chad: You were but
Alicia: we we because I wouldn't allow myself to get to that point because I knew, like, I just viewed his life as, like, an hourglass at this point. Like, we've wasted 3 years now. Like Right. It's like, you know, before Christ, after death. Like, I look at pictures. I'm like, before diagnosis, after diagnosis. Like, we didn't know then. Mhmm. But it's something he was born with. Like, he had it then, and we didn't know. Like Right.
Chad: We
Alicia: were treating ear infections when we should have been treating a terminal illness. Like
Chad: But then it's like, yeah, I just I went into grieving. It just it took a while for me to really just soak it in and realize, like, holy cow. Like, I went through the why us? Like, why is it us? This is you know, why my son? Why this kid? Yeah. You know, he's such a good kid. Like, why you know, the the why's. I went through just an emotional roller coaster of whys. Mhmm. And then I had her, like, I kept asking these whys and, you know, there were answers to them, but it's like I, like, almost couldn't accept it.
Mick Hunt: Right.
Chad: Like, I couldn't accept the fact that I had to wake up with this kid every day and know that that may be the last talk that I might I may get from my boy. Like, for the it probably took me a good 2 years. I mean, a good year or 2. Both 2 years are the longest to like really probably over the last 12 to 14 months is the time frame that I've really like, I don't wanna say end, but accepted. Like, accepted our path, accept what we have to do in our lives to really get where we need to go. Yeah. But also the sport for our daughter because, like, we can't forget her and this whole fact, like Mhmm. You know, she needed us. She needed dad to be supportive and sometimes I wasn't very supportive enough. And it's not I was just feeling my own emotions.
Mick Hunt: Yeah.
Chad: So I didn't really know how to channel my emotions through trying to explain it positively to, well, at that point, 8, 9 year old. I didn't know how to explain it. And you know, sometimes like dad's hide their I can't tell you the number of times I freaking cried on my way to work. I cried in my car and just freaking pulled it together. It's like because I was still working. Like, she immediately at that point
Alicia: Well, he was diagnosed March 2020. So, like, COVID happened like a week later.
Chad: All changing of life happened and then not just of that life in the world was changing, but Right. Our own inner worlds were changing.
Alicia: He could not come to doctor's appointments with me. Yeah. Like, like, when we signed
Chad: one parent.
Alicia: When we signed consent forms for transplant, like Mhmm. He couldn't be there. He had to sign and be on a FaceTime video.
Chad: So it's almost like, yeah. I was grieving, but I almost couldn't accept it because I couldn't be there. So I almost, like I felt like if I was there more, I probably would've been able to establish, like, a feeling better than but I could. I missed out on all of that. She was the one that had to go because I get it. Like, she's the The
Alicia: mama bear.
Chad: Yeah. Like, I get it. So it was like we made that decision, but it it really took me a long time to really establish a feeling of acceptiveness and how I really should feel and attack what we have going with us.
Mick Hunt: Yeah. That's amazing. So mama bear, all the information that's out there, you're seeing 10 years life expectancy, but then you gotta go through the treatments and diagnosis. Right? Walk me through that and then ultimately the decisions that you made with Jacob.
Alicia: So, you know, when we were seen at UNC, they had told us because of his age, because he was 3 and most children are diagnosed either within their first two years of life or through newborn screening, that his brain, for lack of better terms, could be too far gone to go through a bone marrow transplant because the 2, you know, treatment options for this are either weekly infusions of a man made version of the enzyme that he would need once a week for the rest of his life or a bone marrow transplant. And the main difference between the two is that the infusion that he would get does not cross the blood brain barrier. So, eventually, his brain would degrade over time. And, you know, obviously, we want to protect his brain, so we did seek a second opinion through Duke for a bone marrow transplant. And once we went through all of the pretransplant testing, which, you know, looked at every part of his body, you know, his his heart, his lungs, his brain, all of that. They eventually said, you know, he's delayed, but he's not any more delayed than the average 3 year old. So we decided to move forward with a bone marrow transplant, which at the time, you know, they tested our daughter to see if she would be a potential bone marrow match, but we found out in that process that she is also a carrier of this disease. So she they would not use her bone marrow. But they ended up finding a match of cord blood, donated umbilical cord blood. Duke has their own cord blood bank. So they ended up finding a match for him through that. So he had 8 days of chemo. They put a central line in his chest, which is how he would get all of his medicine, how he would get the transplant. And everyone hears transplant and thinks it's like this big climactic experience or procedure and it's really just like a blood transfusion. They delivered these magic cells that were donated, stem cells, from an umbilical cord blood. He had, like I said, 8 days of chemo to hollow out his bone marrow, get rid of all of his cells, and then they infused these stem cells into him, which we were in the hospital for 68 days, but it took him 18 days for his body to what they call engraft, which is take over the donor cells. And the way that that's different from the other treatment option is this will cross the blood brain barrier. So he's making enough of the enzyme now from the donated cells that it will protect his brain and, you know, it's it's not a cure for the disease because he still has 3 years of irreversible damage, but it will slow down the progression of his disease.
Mick Hunt: And are you seeing that?
Alicia: Yeah. I mean, we didn't think he'd ever be potty trained. He's potty trained now. We didn't know if he would ever be able to, like, read.
Chad: Just started writing?
Alicia: Yeah. He just started writing. He just started reading. It's not at the rate of the other kindergarteners that he's around, but it's happening, and we didn't know if that would ever even happen for him. So, you know, those are, like, the small victories that we celebrate. Like, to somebody else, he wrote his name. Like, yeah, yeah. I'm sure it's exciting, but, like, he wrote his name. We didn't know we didn't know if he'd ever used the toilet. Like, that is huge. Yeah. And Yeah. That is because of the transplant, I believe. And I mean, one thing that I know for a fact the transplant helped with is pre transplant testing, he had a sedated hearing test, which showed that he had a moderate to severe hearing loss in both ears requiring hearing aids. We got him hearing aids. Post transplant, his follow-up shows he has normal hearing in both ears.
Chad: They said to get rid of the hearing aids?
Alicia: Yeah. So he does not currently wear hearing aids, and I believe that that's a god thing, but I also believe that, you know, science and
Mick Hunt: Mhmm.
Alicia: And now that he's making this enzyme
Chad: research matters.
Mick Hunt: No. That makes my heart smile. Little guy is gonna be something special. He already is. He's gonna go really And
Alicia: like I said like I say all the time because I've had people say, like, you know, what if this doesn't help him? Like, what if a cure is not found in his lifetime? Or what if you're putting in all of his advocacy and it's not gonna help him? It might not help him, but he's a part of it. His purpose. Yeah. He still has purpose. His life still means something even if it's helping the future babies.
Mick Hunt: That's awesome. Let's talk about Jacob now. So what's that journey been like for the last 4 years?
Alicia: So since transplant, he had some complications during transplant, but he did great with it all things considered. We overcame all of those. He has had multiple surgeries since then. He's had bilateral carpal tunnel repair. He's had decompression infusion of his cervical spine. He's had bilateral hip reconstruction and plates put in his knees. He's continuously followed
Chad: after for like, what, 6 months, 6 to 8 months?
Alicia: We were doing like home, we were doing like home infusion.
Chad: He had a t tube in his belly at the same time. So he had literally 2 things that are ordered in his body for 6 to 8 months post transplant.
Alicia: But he is the happiest.
Chad: Mhmm.
Alicia: Like, he is inspiring.
Mick Hunt: That's awesome.
Alicia: He takes everything with stride. And that's why it's so important for us because it's all relative. Right? Yep. When your kid gets strep, if that's the biggest thing happening in your life, like, that's gonna feel terrible to you. How like, your kid is sick. You wanna do everything you can make them better. Mhmm. And before all of this, our issues were so
Mick Hunt: small.
Alicia: Right. Whereas now, we've had to, like, shift and think, like, how lucky we are. Correct. Because I personally know other families who went through transplant with us that didn't bring their kids home. Mhmm. Mhmm.
Chad: And we were told that risk from the beginning. They're like, listen. This is a risk but
Alicia: It's a risk we took to not even be able to save his life.
Chad: It's like relative to people in life. Like, it's not like sitting at a poker table or anything in life. Like, anyone watching take a relative risk of what you think you took in life and then put it in our shoes and bring it in your children's life and like hey.
Alicia: That's not that's not downplaying other people's problems. No. Like, that's like
Chad: bring it relative to the decisions that we all make in lives. Like, it was probably ultimately one of the hardest decisions, like, we ever had to make in life.
Mick Hunt: Yeah. And so you talked about essentially saying your outlook on life is drastically different
Alicia: now. Yes.
Mick Hunt: Moments matter. I'm I'm not saying moments never matter.
Alicia: Right.
Mick Hunt: But the appreciation for minutes of the day Mhmm. Have to be different for you now. Right? Talk to me a little bit about just your outlook on life and how that's changed.
Alicia: So I definitely am a silver lining type of person. I've had to retrain my brain to think that way.
Chad: 1st, I'm I'm a very momental person.
Alicia: If I don't, like, I am very high anxiety. Like, I carry a lot of stress and and a lot of anxiety. And people, like, tell us all the time, like, you're so strong. And it's like, I'm not strong because I'm I want to be strong. Like, I wish I didn't have to be strong,
Chad: like Right.
Alicia: All of the time. Right. But I don't have enough choice. Like, if you have a child and you were in my shoes, you would be doing the exact same thing. I'm not special. Like, we are not any different than anybody else. Like, we were dealt a not great hand, but we have to be able to take that and turn it into something positive. And, you know, like I said, we've advocated. I've met virtually because everything is virtual now, but with North Carolina legislators and, you know, we've gotten newborn screening passed for the state of North Carolina. As of February of last year, any baby born in the state of North Carolina is tested for MPS one at birth.
Mick Hunt: That is freaking
Chad: awesome. Yeah. Yeah.
Alicia: So and I mean, that was not solely because of me. You know, the MPS Society exists and they're out of Durham, oddly enough. They happen to be super close to home for us. Okay. So very involved with them and all of the work and research and everything that they do. But
Chad: Now piggybacking on what you said before about the grieving dad. Mhmm. There was a turning point for me. Like, where she's very stressful, high anxiety, she gets through it. She was tough at the beginning. It's like almost shifted. Like, I'm the more memento person. I'm like, she is there and we have so much fun, but I'm like I'm now kinda like, I'm not gonna miss out on things. Like, I'm in the restaurant world. That's how I'm saying that.
Mick Hunt: Right.
Chad: You know? And there was actually even sacrifices that I made during his diagnosis. And while they were in the hospital, like, I missed out on fundraisers things. And it was sad, but it was the sacrifice that we had to make to get where we needed to go. I mean, right now, obviously, we're doing this podcast in the middle of my restaurant's dining room and it's awesome and we're blessed to feel like we're here right now. But there was definitely a turning point for me mindset wise where I just like clicked.
Alicia: Had to prioritize the time that we do have with our team.
Chad: Yeah. I mean I can probably think about it. It was like the very end of 2022. So you're talking almost 2 years. Like I don't know what it was. There was just a moment in my head that just I flipped the switch.
Mick Hunt: Flipped it. Right.
Chad: But I also have brought that to, like, my work life, just my personal life. Like, tell people this and people that know me and work for me and everyone that knows me. Like, I always say Jacob's diagnosis has been a cheat code delight for me because it really taught me how to just be in the moment. We all have accolades we wanna chase. We all have goals and dreams and I did. Like, we all do. Everyone had every single thing that they wanted to reach for something. And, you know, you wanna reach those stars. And I kinda had to like set that aside.
Alicia: And
Chad: just the moment of feelings that people have in life goals and jobs and careers and sports, like, for me, that was all I had. And now I kinda like reshifted my mindset. I've told people I don't care what it is. Like I'm not gonna miss out on a moment with my kids anymore. Like doesn't mean sports or a job or anything. Nothing will come in between having that momental moment because as she has reiterated many of times, that moment may may never happen again. Right. I tell people, like, the best thing that I do every day is I wake up in the morning. We hear this kid going, Dada, mama, get me out of my room. Like
Alicia: And going back to, like, the perspective shift, he has some behavioral issues, and he has, like, some
Chad: things. Well, what what I wanted to say was, like, the best thing every day is I start our day by being able to hug this kid. Mhmm. Because and I actually wake up every morning just knowing that's what I want because nothing else matters.
Mick Hunt: Right.
Chad: My restaurant, my job, sports that I play, I'm big into golf. Like nothing matters besides getting that hug from the whole of our kids obviously but the one you know, Jacob especially because that's what we're talking about. But and then it it actually, like, carries to the rest of my day. Nothing else can matter. Somebody can give me the worst news ever and I literally looked at them and I go, it's okay. Right. Because let me help you through that because we have been through that raw emotion of people telling us like it's okay. I feel like and we have like a gift to give to people.
Mick Hunt: Yeah.
Chad: They can look at us, and I will find the positivity in anything now just because of what we went through in life so far.
Mick Hunt: No. I love that. And then you were talking about the behavioral issues. Right?
Alicia: I was just gonna say, like, a shift in perspective. Like, some of the things that take place aren't pleasant all of the time, and we still have to be able to discipline just like we discipline our daughter. Like, it's no different. But at the same time, it's like, oh, that really bothered me. But at the same time, there are parents wishing that their kids would stand on the table and dump cheerioza. And they're not awarded they don't have that. So it's we have to be able to make that shift. And this diagnosis is definitely gonna make our daughter a more compassionate, inclusive adult
Chad: Mhmm.
Alicia: Because she's exposed to so much more, which has its positives and its negatives. I mean, not that she's had to grow up quicker, but she's seen and heard a lot of traumatic and real life things, and we don't keep that from her. Like, nobody knows how long anybody has,
Chad: and
Alicia: it's not something we think about on a daily basis.
Mick Hunt: Right.
Chad: But it's
Alicia: always there. I mean Mhmm.
Chad: It's
Alicia: something we think about, and we take into consideration when we're making decisions and things like that. But we also have a really great community, like, within the MPS community. Like, I'm connected with a bunch of other moms. We vacation together. We are each other's support system because nobody does a good job.
Chad: Every year.
Alicia: There's a conference every year. Okay. Nobody really knows what it's like unless you're in it. You know?
Mick Hunt: So let's talk about some of the advocacy for MPS 1. And you said, Chad, there's SEP so not just MPS 1, but MPS 1 through 7, I'm assuming?
Alicia: There's there's multiple types and ML, which falls under. It's the National MPS Society, but they support and advocate for all types of MPS and ML Okay. Which MPS stands for mucopolysaccharidosis, which is just a really long
Mick Hunt: Yes.
Alicia: Scientific name and then ML is mucolipidosis.
Mick Hunt: And I can't say either of those 2, so I'm gonna say
Chad: MPL at the beginning. I said I told them the acronym, and I said my wife can perfectly explain the full name Yeah. Every single time.
Mick Hunt: There we go. So how can people join and fight the cause? Because number 1, I need to commend you for fighting. Even though you say it wasn't you that got North Carolina legislature to approve it, but someone had to start.
Alicia: Yeah.
Mick Hunt: Someone had to be the carrier of the voice. And I will say that you were that megaphone. So number 1, kudos to you for that.
Alicia: Thank you.
Mick Hunt: But what are things that people can be doing to help support this? Because just like a lot of other diseases where there's researching, that all takes money. That all takes awareness. What can we do to support this?
Alicia: So things that anybody can do, you can join Be The Match as a bone marrow donor because somebody out there or, you know, if you're pregnant or you know somebody who's pregnant, you can donate your umbilical cord blood because that's just going to be used as medical waste. And because some selfless mother out there decided to donate her child's umbilical court, our child gets a second chance at life, which literally costs you no money. You can sign up, like I said, be the match to be on the bone marrow registry. The chances that you'll ever be called to be a donor is very, very slim, but you could and you could change somebody's life. You know, you can donate to either the National MPS Society or the Kennedy Lab Foundation. Those are both 2 nonprofit organizations that fund research. You can follow us on Facebook.
Chad: Jacob's Journey?
Alicia: Yeah. It's Jacob's Journey with MPS 1.
Chad: We do multiple fundraisers.
Alicia: It's more posting updates on how he's doing and then glimpse into our life and the things that he goes through on a daily basis.
Chad: But you put a lot of fundraisers together.
Alicia: Yeah. We do multiple fundraisers a year whether it's a t shirt drive or we just did one for a custom pair of shoes. But
Chad: Parks are customs, by the way. There you go.
Mick Hunt: There you go.
Alicia: But, really, you know, just raising awareness to us is so important. Like, this opportunity for us to reach however many more people that we wouldn't heard of before because even the awareness portion of it, whether it reaches a high school student who knows they wanna go into science and research, but they don't know what they wanna do. Mhmm. Maybe this is a possibility. This is an outlet for them. Maybe somebody is gonna see this podcast who has a child with all of these symptoms that Jacob had, and they don't know it. Like, I personally know people who have been diagnosed because somebody approached them in a mall and said, your child looks like somebody that I know who has this disease. Like, that literally changed
Chad: She's called me multiple times.
Alicia: The whole course of their life. Life. Like Yeah. And, you know I just
Chad: look at the significance too. Like, we're sitting here with on mixed podcast, and this gentleman just happened to walk into my restaurant one night and to eat dinner, and we just got to conversating about life and, you know, podcasts. And I brought it up to you, and I was like, let's do it. You know what I mean? I I just feel like all walks of life, we all take it for granted all the time.
Alicia: Well, and like you said, going back to, like, research, like, ultimately, funding is what's holding our child back from having a future. Okay. Like, this is considered an orphan disease. Pharmaceutical companies aren't researching treatments for diseases that aren't going to make them money because this does not apply to the masses. There are not 1,000 and 1,000 and millions of people who have this, they're not gonna make money off of this, which as disgusting and sad as that is, that's the truth.
Chad: So Yeah. We have to walk it.
Alicia: So we have to be the advocates. We have to be the people to raise the money, to fund the research, to because it affects us. And we didn't for the 1st 3 years of his life, we didn't know. Like, we were just normal people who had normal kids and lived a normal life, and one day, that all changed for us. And that could happen to anybody.
Mick Hunt: It it totally can. And for anyone that's listening or that's watching, this is why donation matters. And and this is why simple things like donating and build. Right?
Alicia: Yeah.
Mick Hunt: All this matters because without this, the life expectancy is 10 years old.
Alicia: That's outdated information. It is longer than that. And that's the That's
Chad: with no medical treatment.
Mick Hunt: But but that's what I'm saying. Right. Yeah.
Alicia: And that's the scary thing. When you get on, like, that information stops your art. Like, that's like How
Chad: many families out there in the world get diagnosed with this that can't go through clinical treatment? And they just literally have to watch their kids just wash away.
Mick Hunt: And and that's what I mean. So we all have kids, have nieces, have nephews, have cousins, whatever it is. Life is so precious. And if there's anything that you can do, please do it, because all of this matters. The most precious thing that we have is life, and the second most precious thing that we have is time. Donating for research and for funding can allow both of those things to happen. And so from my heart to both yours, number 1, I appreciate you taking the time to be here. We
Chad: appreciate it.
Mick Hunt: But if there's anything that you want the listeners or viewers to end with, if there's one last message that you want them to have, what would
Chad: that be? Let me start.
Alicia: Hug your kids. Every moment with them is precious whether they have any diagnosis. And, you know, teach your kids about inclusion. Teach them to not stare, to ask, to say hi, to, you know, to engage with other kids. You know, that's my biggest fear because he is going to continue to be different. Like, this is a degenerative and progressive disease. Mhmm. And I just want him to be happy.
Mick Hunt: There you
Alicia: go. Like, happiness is what matters.
Chad: That's right. I'll piggyback on that. I mean, yeah, hug your loved ones, your kids, like, those moments just they may not ever be there. So And it
Alicia: not everybody has the means to donate, and I totally understand that. And even those who have supported us and donated, like, donor burnout is real. Like, we are constantly asking for people to donate. And a share of this podcast, a share of a Facebook post, like I said, we had never heard of this.
Mick Hunt: Yeah.
Alicia: Just talking about it, that's helping us. That's helping future families. That's helping future babies. All of that matters. And it doesn't need to be this $1,000,000 donation.
Mick Hunt: Yeah. But if 2,000,000 people all gave a dollar, what does that do? And and that's what I want people to understand. And in the links in the description, you're gonna see a lot of ways that you can donate. Just choose something. I promise. And it doesn't matter if it's a dollar. It doesn't matter if it's 5. Like, something goes a long way. And so for me, that's my one ask, is that everyone donate in your own way, in your special way. Because there are a lot of Jacob's, and there are a lot of mothers and fathers of Jacob's that truly would appreciate it. Would you agree?
Chad: I understand.
Mick Hunt: For all the listeners and viewers, remember, your Because is your superpower. Go on, Jason.
Intro: Thanks for listening to Mick Unplugged. We hope this episode helps you take the next step toward the extraordinary and launches a revolution in your life. Don't forget to rate and review the podcast, and be sure to check us out on YouTube at Mick Unplugged. Remember, stay empowered, stay inspired, and stay unplugged.

 Mick Hunt
Mick Hunt

![Justin Benton | Challenge to Triumph: Harnessing the Power of Hemp for Health - Mick Unplugged [EP 28]](https://mickunplugged.com/hubfs/YT%20%20Thumbnail%20-%20EP28.png)
![Lauren Sisler | Resilience on the Sidelines: Journey of Personal Triumph- Mick Unplugged [EP 31]](https://mickunplugged.com/hubfs/YT%20Thumbnail%20-%20EP31.jpg)
![Sandy Kruse | Rising from the Ashes: A Journey of Health and Healing - Mick Unplugged [EP 38]](https://mickunplugged.com/hubfs/unnamed%20%281%29.jpg)